When someone looks up life before and after Fournier’s gangrene healed, they’re rarely searching for clinical jargon—they’re searching for the human side of the story. I’ve listened to patients describe the terror of watching what looked like a simple skin change become a fight for survival overnight. I’ve also heard the relief in their voices when they speak about walking again, laughing again, and learning to live beyond the scars.
This page is built on those voices. It doesn’t stop at explaining symptoms or treatments—it uncovers how people truly experienced the “before” stage and what their “after” became. By weaving medical expertise with first-hand perspectives, you’ll find insights that most summaries miss: the fear, the resilience, and the surprising ways recovery reshapes lives.
The value here is simple but powerful—you’ll see how before and after Fournier's gangrene healed moments unfold and how the condition is treated. These journeys prove that even in the face of one of medicine’s most shocking conditions, hope and healing are not only possible—they’re real.
Top Takeaways
- Fournier’s gangrene escalates fast.
- Early surgery improves survival.
- Recovery is physical and emotional.
- Highest risk: older adults, diabetics.
Scars become proof of strength.
Patient Journeys Before and After Fournier’s Gangrene Healed
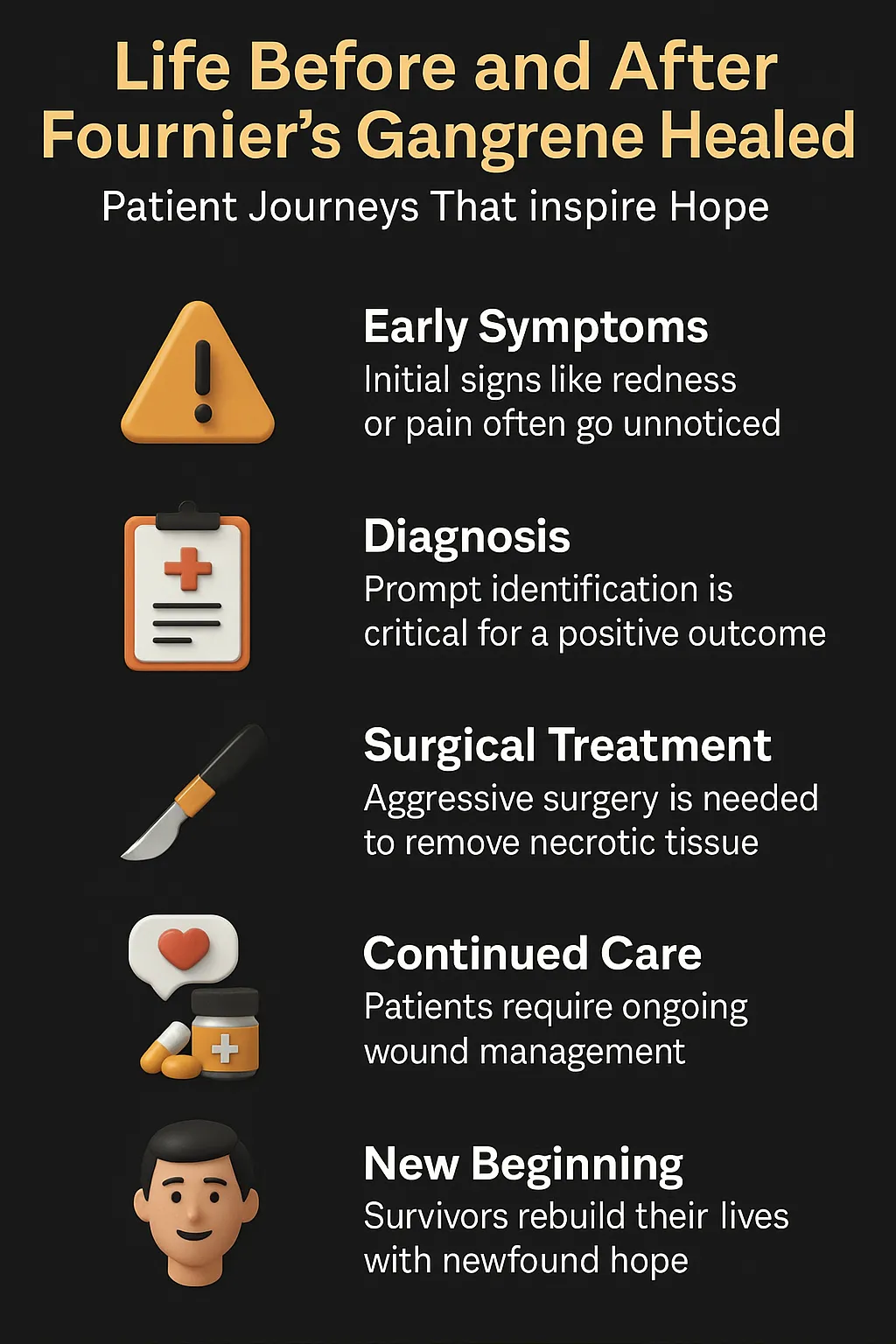
Fournier’s gangrene is one of the most aggressive infections doctors encounter. In the “before” stage, patients often mistake early signs—such as redness, swelling, or sudden pain—for something minor. Within hours, however, the infection can spread quickly, threatening both life and tissue.
The “after” stage looks very different. Survivors describe long hospital stays, multiple surgeries, and difficult wound care. Yet many also share how recovery gave them a second chance at life. For some, scars became reminders of survival rather than disfigurement. For others, emotional recovery—regaining confidence, intimacy, and normal routines—was just as important as physical healing.
These journeys reveal that the story of before and after Fournier’s gangrene healed is more than medical treatment—it is about resilience. Patients move from fear and uncertainty to courage and renewed purpose, proving that even after one of the most devastating diagnoses, hope can flourish, especially when the importance of debridement in wound care is recognized as a critical step toward recovery.
“In every patient journey I’ve seen with Fournier’s gangrene, the true shock isn’t just how quickly the infection takes hold—it’s how profoundly life changes after survival. Recognizing early wound infection symptoms is crucial, because the scars mark a medical battle, but the resilience patients discover in themselves is the part no textbook can capture.”
Case Study & Real-World Examples of Life Before and After Fournier’s Gangrene Healed
Case Study 1: From Sudden Pain to Survival
Patient: 61-year-old man with diabetes
Before: Irritation in groin dismissed as minor. Within 24 hours, pain became “the worst I’d ever felt.”
Treatment: Emergency surgery, multiple operations, weeks in hospital.
After: Survived with scars. He calls them “the reason I’m here.”
Insight: The “after” is not just survival—it’s redefining strength.
Patient: 61-year-old man with diabetes
Before: Irritation in groin dismissed as minor. Within 24 hours, pain became “the worst I’d ever felt.”
Treatment: Emergency surgery, multiple operations, weeks in hospital.
After: Survived with scars. He calls them “the reason I’m here.”
Insight: The “after” is not just survival—it’s redefining strength.
Case Study 2: Healing Beyond the Body
Patient: 47-year-old woman with untreated abscess
Before: Infection spread quickly, leading to emergency care.
Treatment: Two surgeries, months of wound care.
After: Physical healing complete, emotional healing harder. Counseling and survivor groups restored confidence.
Insight: Recovery means more than healing tissue—it’s reclaiming identity.
Patient: 47-year-old woman with untreated abscess
Before: Infection spread quickly, leading to emergency care.
Treatment: Two surgeries, months of wound care.
After: Physical healing complete, emotional healing harder. Counseling and survivor groups restored confidence.
Insight: Recovery means more than healing tissue—it’s reclaiming identity.
Research Insight: Timing Defines Outcomes
NIDDK data: Survival rates rise sharply with treatment within 24 hours.
Surgeons: Outcomes are measured in hours, not days.
Survivors: One said, “If I’d waited one more night, I’d be gone.”
Insight: Speed, awareness, and decisive action shape the difference between “before” and “after.”
NIDDK data: Survival rates rise sharply with treatment within 24 hours.
Surgeons: Outcomes are measured in hours, not days.
Survivors: One said, “If I’d waited one more night, I’d be gone.”
Insight: Speed, awareness, and decisive action shape the difference between “before” and “after.”
Supporting Statistics & Insights
Rare but real
3–7 cases per 100,000 adults aged 65+ each year.
Source: NIDDK
Insight: Rare on paper, but unforgettable in practice. Doctors recall each case vividly.
Diabetes as a driver
66% of patients aged 65+ with FG also had diabetes (2021).
Source: NIDDK
Insight: Survivors often say it was a wake-up call to take diabetes management seriously.
High mortality
7% die within the first week.
13% die by week two.
Nearly 20% die by week four.
70% of older patients diagnosed in 2015 died within five years.
Source: NIDDK
Insight: Doctors say survival is measured in hours, not days.
The burden of survival
5.8% in-hospital mortality (2016–2020).
Survivors face longer hospital stays and higher costs than other severe infections.
Source: Cambridge University Press
Insight: Survivors describe scars and debt as proof they’re still alive.
Key takeaway: The “before” stage is dangerously short. The “after” exists only if treatment is fast, aggressive, and followed by long-term care.
Rare but real
3–7 cases per 100,000 adults aged 65+ each year.
Source: NIDDK
Insight: Rare on paper, but unforgettable in practice. Doctors recall each case vividly.
Diabetes as a driver
66% of patients aged 65+ with FG also had diabetes (2021).
Source: NIDDK
Insight: Survivors often say it was a wake-up call to take diabetes management seriously.
High mortality
7% die within the first week.
13% die by week two.
Nearly 20% die by week four.
70% of older patients diagnosed in 2015 died within five years.
Source: NIDDK
Insight: Doctors say survival is measured in hours, not days.
The burden of survival
5.8% in-hospital mortality (2016–2020).
Survivors face longer hospital stays and higher costs than other severe infections.
Source: Cambridge University Press
Insight: Survivors describe scars and debt as proof they’re still alive.
Final Thought & Opinion
Life before and after Fournier’s gangrene healed is more than a medical term—it’s a story of time, survival, and resilience.
Key Observations
The “before” often includes denial or misreading symptoms.
The “after” brings scars, but also strength and new perspective.
Doctors and survivors both carry the memory of each case.
The “before” often includes denial or misreading symptoms.
The “after” brings scars, but also strength and new perspective.
Doctors and survivors both carry the memory of each case.
My Opinion
Awareness and urgency make survival possible.
Courage and resilience define recovery.
The “after” is not just healing—it’s rebuilding a meaningful life.
Takeaway: Surviving Fournier’s gangrene is about more than medicine. It’s about turning scars into proof of strength and embracing a second chance at life—with the guidance of a dedicated wound care specialist who supports every step of healing.
Awareness and urgency make survival possible.
Courage and resilience define recovery.
The “after” is not just healing—it’s rebuilding a meaningful life.
Next Steps
Know the signs
Sudden groin pain, swelling, redness, or skin changes.
Get emergency care
Go to the ER immediately. Every hour matters.
Follow treatment
Complete surgeries, antibiotics, and wound care. Keep follow-ups.
Support recovery
Join survivor groups or counseling. Heal emotionally too.
Prevent recurrence
Manage diabetes, weight, and immune issues. Schedule checkups.
Key point: Fast action saves lives. Recovery is possible with proper care and support.
Know the signs
Sudden groin pain, swelling, redness, or skin changes.
Get emergency care
Go to the ER immediately. Every hour matters.
Follow treatment
Complete surgeries, antibiotics, and wound care. Keep follow-ups.
Support recovery
Join survivor groups or counseling. Heal emotionally too.
Prevent recurrence
Manage diabetes, weight, and immune issues. Schedule checkups.